Latest Insights and Updates
Stay informed with our latest articles.
In the Post-Pandemic COVID-19 Era, Nursing Homes Remain Vulnerable
Analysis of current COVID-19 trends in nursing homes, showing increased vulnerability despite lower overall death rates. Discusses vaccination rate declines, rising infection rates, and the importance of continued vigilance in long-term care facilities.
In the post-pandemic era, it is tempting to let out a big sigh of relief and try to return to "business as usual." Unfortunately, the world has forever changed in some ways, and for our most vulnerable populations, the threat remains. The elderly, those with chronic illnesses and disabilities, and the very young are at a higher risk than average.
None of us want to go back to the pandemic when we watched with a sense of dread as infection rates and maps on our televisions updated daily - but it's not prudent to ignore new surges in COVID infections either. The latest COVID variants have been ramping up in some areas in 2024, posing a threat to the most susceptible.
What Does the Data Say?
The most common sources for COVID-19 data and trends are the CDC and the WHO. When looking at a provisional COVID-19 deaths-by-week graph spanning 2020 to the present, it is obvious that we are over the worst of it. At it's peak in 2020, deaths topped 25,000 per week. September 2024, so far, is now reflecting around 1,100 deaths per week.

As you can see, COVID-19 is still peaking, with around two peaks per year. We are currently in the first peak of 2024-2025. If the pattern holds true, we can look forward to another one in a few months.
Of note, this graph reflects only deaths, not infections or hospitalizations. Those numbers are a bit more difficult to validate, due to the availability of self-testing kits, comorbid conditions in the hospital, and other factors. What we DO know from historical data is that nursing home resident deaths typically exceed the death rate of the general population. During the heat of the pandemic, nursing homes reported over 25 times the death rate reported in the general population.
Why Are Nursing Homes Vulnerable?
Common sense tells us that residents of nursing homes are typically cared for in a clean facility, with greater attention to infection control than other public places. However, congregate living situations, staff exposure from outside the facility, and depleted immune systems from chronic conditions and age form a troublesome mix of risk factors. Another worrisome fact is the extreme speed at which a wave of Coronavirus can spread within a facility.
Vaccination Rates on the Decline
As we see in the trends above, COVID-19 cases and deaths began to climb again. The AARP published its own warning based on an analysis of federal data - we are in for a rough winter. The virus has a pattern of surging around the holidays, and this year's case and death rates are tracking higher than last year. Additionally, less attention is being given to getting COVID-19 boosters - both by LTC residents and staff.
AARP's senior methods advisor Ari Houser states "It is critically important that nursing home residents and staff get vaccinated during the fall to achieve maximum protection for both themselves and all residents living in the facility."
Infection Rates on the Rise
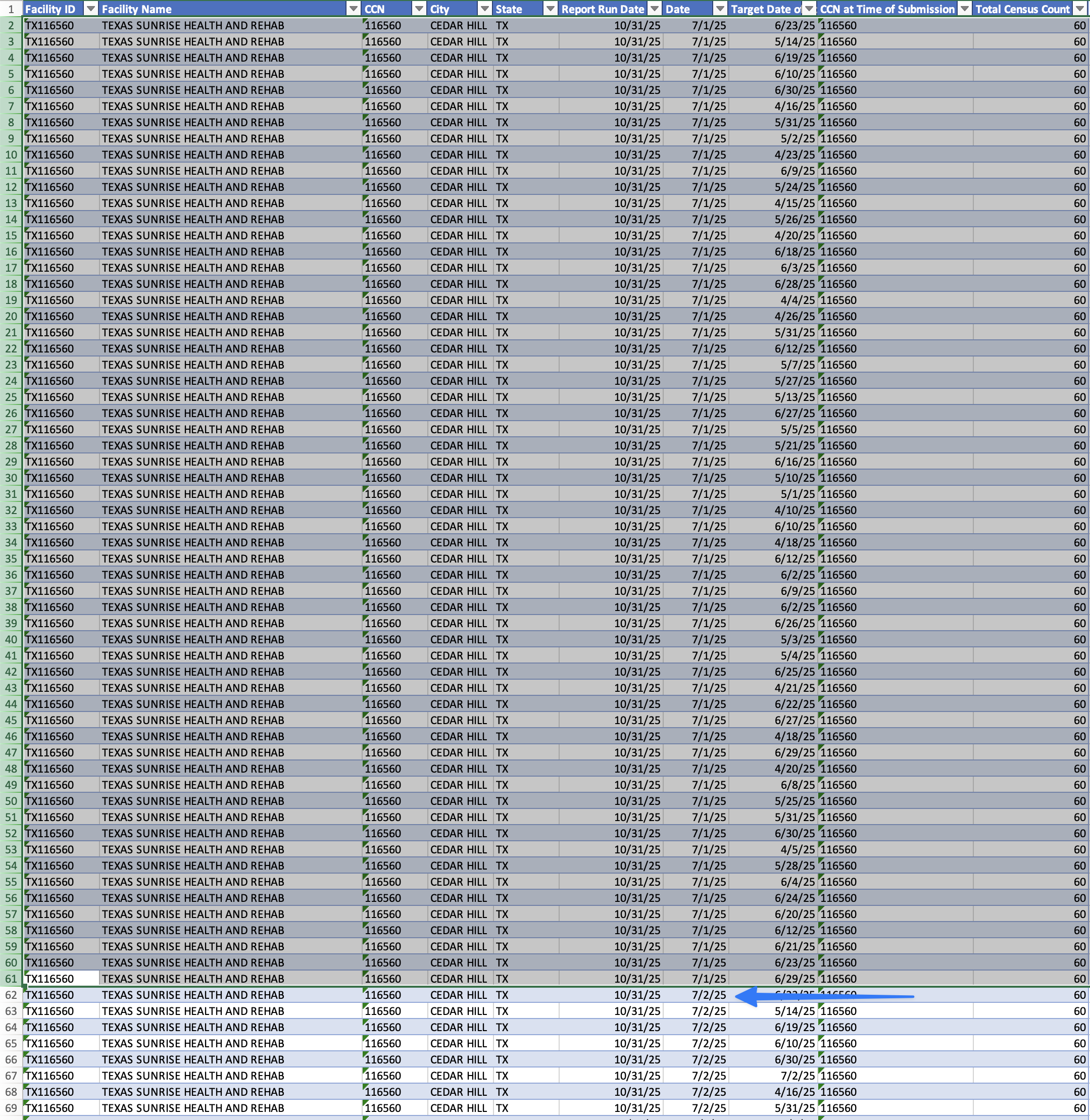
When looking at recent data from 2024 collected from nursing homes, the trends are concerning.
- During the period from July 29 to August 25, the rates of resident and staff COVID cases increased by seven fold compared to the four weeks ending May 26.
- One out of every 28 nursing home residents tested positive for COVID-19 during the latest monthly period.
- Resident deaths from Coronavirus increased five times, jumping from 100 in the period ending in May, to 500 for the month ending August 25.
Vaccinate and Report - Easy, right?
When it comes to the raw data, nursing home facility data is some of the most accurate, due to mandated reporting. This accuracy comes at a price for many facilities that are struggling to find staff and balance workloads. If your facility could use a partner to ensure timely and accurate COVID-19 vaccination and case reporting to NHSN, Votive could be the partner you are looking for. Votive's experience throughout the pandemic has refined our methods for collecting data and submitting it on your behalf to the CDC and CMS. Avoid threats of fines, and time-consuming data gathering, while you rest easier with a partner dedicated to your success.
What's New in 2024 with the Resident Assessment Instrument (RAI)
Overview of key updates to MDS 3.0 RAI User's Manual version 1.19.1, effective October 2024. Highlights new items for anticonvulsant medications and COVID-19 vaccination status, removal of discharge goals columns, and expanded guidance on assessment corrections.
The final Minimum Data Set (MDS) 3.0 Resident Assessment Instrument User’s Manual (version 1.19.1) is available as of August 1, 2024. What are the need-to-know changes that can impact your facility?
New Changes to the MDS Resident Assessment Instrument in 2024
The Centers for Medicare & Medicaid Services (CMS) has released significant updates to the Minimum Data Set (MDS) 3.0 Resident Assessment Instrument (RAI) User’s Manual, effective October 1, 2024. These changes aim to enhance the accuracy and efficiency of resident assessments in nursing homes and other long-term care facilities. Here are the key updates:
Five Changes to Know:
- Two new items have been introduced:
- N0415K: Anticonvulsant – This item captures information about residents’ use of anticonvulsant medications
- Various minor adjustments have been made throughout the manual to clarify existing guidelines and ensure consistency. These include updates to examples and explanations in different sections. – This item records whether a resident’s COVID-19 vaccination is up to date.
- Removal of Discharge Goals Column:
The Discharge Goals column has been removed from some sections. This change is intended to streamline the assessment process and reduce the burden on healthcare providers. This applies to the following sections:- GG0130: Self-Care
- GG0170: Mobility
- Expanded Guidance on Manual Assessment Correction/Deletion Requests:
The manual now includes more detailed instructions on how to submit and correct assessments. These updates aim to improve the accuracy of resident data and ensure that corrections are handled efficiently. This expanded guidance is found in:- Chapter 3, Section X
- Chapter 5
- Minor Alignments and Clarifications
Various minor adjustments have been made throughout the manual to clarify existing guidelines and ensure consistency. These include updates to examples and explanations in different sections.
- Hyperlink Update Supplement
- A new supplement has been added to the manual to ensure that all hyperlinks remain current. This document lists non-functional or outdated links and provides up-to-date replacements.
Implications for Healthcare Providers
These updates are designed to improve the quality of resident assessments and ensure that healthcare providers have the most accurate and up-to-date information. CMS aims to reduce the administrative burden on staff while enhancing the overall care provided to residents by streamlining certain processes and adding new items.
Healthcare providers should familiarize themselves with these changes and update their assessment procedures accordingly. Training sessions and workshops may be beneficial to ensure that all staff members are aware of and understand the new guidelines. Providing up-to-date COVID-19 vaccination information remains a priority, and should be a focus for facilities at several reporting levels.
Conclusion
The 2024 updates to the MDS 3.0 RAI User’s Manual reflect CMS’s ongoing commitment to improving the quality of care in long-term care facilities. By incorporating new items, removing redundant columns, and providing expanded guidance, these changes aim to make the assessment process more efficient and accurate.
For more detailed information, healthcare providers can refer to the full MDS 3.0 RAI User’s Manual available on the CMS website12.
Nursing Home Minimum Staffing Standards - Implementation Details to Know
Detailed explanation of CMS's new nursing home staffing requirements, including 3.48 HPRD standard implementation timeline, temporary exemptions for rural facilities, and facility assessment requirements. Outlines three-phase implementation process through 2024-2025.
The hotly contested minimum staffing requirement for nursing homes is set to take effect. What does implementation look like for facilities?
On April 22, 2024, CMS affirmed its commitment to hold nursing homes accountable for providing safe staffing levels and high-quality care for its nearly 1.2 million Medicare and Medicaid beneficiary residents. The CMS rule finalizes a total nurse staffing standard of 3.48 hours per resident day (HPRD), which must include at least 0.55 HPRD of registered nurse care and 2.45 HPRD of direct nurse aide care. Facilities may use any combination of nursing staff (RN, LPN/LVN, and nurse aides) to account for the additional 0.48 HPRD staffing standard.
Temporary Exemptions
Some rural facilities and others experiencing staffing hardships may apply for temporary exemptions and a delayed implementation, in recognition of the known issues some facilities are experiencing.
Staggered Implementation Schedule
While to some the nursing home minimum staffing standards don't seem that difficult, it does represent a challenge for many organizations to recruit enough staff and operationalize their processes to stay compliant.
Phase 1 - Within 90 days of the final rule publication, facilities must meet the facility assessment requirements.
Phase 2 - Within two years of the final rule publication, facilities must meet the 3.48 HPRD total nurse staffing requirement, and the 24/7 RN requirement.
Phase 3 - Within three years of the final rule publication, facilities must meet the 0.55 RN and 2.45 NA HPRD requirements.
The Patient Needs Assessment
The minimum standard requirements are more than about hitting numbers - facilities must use evidence-based methods when care planning and implement those special patient needs into the staffing plan. The staffing plan should not only be tailored to fit the needs of the current patient population, but updated often as those needs change. Learn more about patient needs assessments and evidence-based tools to support staffing decisions.
Is your organization ready to hit these targets? Now is the time to start planning and exploring ways to put the staffing and reporting pieces into place. Votive is an expert in LTC reporting, and is here to help lift the heavy load. Contact us for more information and a free demonstration to learn how we can assist.
Get Ready Now - NHSN Changes COVID-19 Reporting for Q4 2024
NHSN announces significant changes to COVID-19 reporting requirements starting Q4 2024, including new definition of 'up to date' vaccination status, introduction of combined respiratory pathogen reporting form, and retirement of Pathway Data Reporting form.
Changes to take effect Sept 30, 2024
The National Healthcare Safety Network (NHSN) has announced several important changes to COVID-19 reporting that will take effect in the fourth quarter of 2024. These updates aim to streamline data collection and improve the accuracy of reporting for long-term care facilities and hospitals. Here are the key changes:
- Updated Definition for “Up to Date” COVID-19 Vaccination
- Starting September 30, 2024, the definition of “up to date” for COVID-19 vaccination will change. An individual will be considered up to date if they have received a single dose of the 2024-2025 updated COVID-19 vaccine. Until this vaccine is administered, facilities should report zero individuals as up to date.
- New Combined Respiratory Pathogen Reporting Form
- Facilities will need to use a new combined reporting form for respiratory pathogen vaccination, case, and hospitalization data. This form will replace the existing Pathway Data Reporting form for positive COVID-19, influenza, and RSV cases. While COVID-19 reporting remains mandatory, reporting for influenza and RSV will be optional.
- Retirement of the Pathway Data Reporting Form
- The existing Pathway Data Reporting form will be retired and archived. This change is part of the effort to consolidate and simplify the reporting process.
- Webinars and Training Sessions
- To help facilities transition to the new reporting requirements, NHSN will host a series of webinars. These sessions will cover the updates to the resident data collection form and the new definition for up-to-date COVID-19 vaccination reporting.
Implications for Healthcare Providers
For Long-Term Care Facilities:
- Training Needs: Staff will need to be trained on the new reporting requirements and the updated definition of “up to date” vaccination.
- Data Collection: The new combined form will streamline data collection, but staff will need to ensure they are accurately reporting all required information.
- Administrative Adjustments: Facilities may need to update their internal processes and electronic health record (EHR) systems to accommodate the new reporting form.
For Hospitals:
- New Reporting Requirements: Starting November 1, 2024, hospitals will be required to electronically report information about COVID-19, influenza, and RSV as part of the CMS Conditions of Participation.
Need Help?
We know that NHSN reporting can be time-consuming and frustrating. That is why Votive partners with post-acute care providers to ensure timely reporting, and accuracy while freeing up valuable staff time for caregiving. Want to know more? Contact us for a free demo and answers to your questions.
Trusted by Healthcare Leaders
Votive transforms compliance processes completely
Stay Updated with Our News
Subscribe to our newsletter for the latest updates and insights in post-acute healthcare.
Frequently Asked Questions
Find answers to common questions about us and our product
What is Votive?

We’ve built Votive for post-acute healthcare providers - skilled nursing facilities, home health agencies, and rehab centers. If your team needs an easier way to manage compliance and reporting, we’ve got you covered. Our platform is simple to use, adaptable to different care settings, and designed to take the stress out of staying compliant.
How does it work?

We keep it simple. Choose the tools your facility needs - PBJ reporting, NHSN reporting, or both - and we’ll guide you through setup from start to finish. Our team handles the heavy lifting so you can start streamlining compliance without disrupting your workflow.
Who can use it?

Our tools are built for the whole team, from administrators and compliance officers to schedulers and nurses on the floor. If your role touches staffing, reporting, or compliance, we’re here to make your job easier.
Is training included?

Absolutely. We guide your entire facility through onboarding and provide hands-on training to help your team get the most out of our tools. We make sure everyone knows how to use the features that matter most to you.
How to get started?

It’s easy. Just book a call on our demo page, and one of our team members will walk you through a personalized demo and help you get set up with the platform.